Health Plan Capabilities
Extract, aggregate and standardize member data for a longitudinal view with Exchange Nexus, an end-to-end interoperability solution for health plans.
Health Plans struggle to acquire the data necessary to effectively manage their network.
Challenges abound, including disparate electronic medical records (EMRs), numerous data standards, and identification of necessary data points—all costly and time-consuming. Our solutions simplify data exchange, reducing provider abrasion and vendor complexities. Discover the efficiency of an integrated approach that enhances data accessibility and insights, paving the way for more informed healthcare decisions.

LATEST NEWS
MRO has earned the Validated Data Stream designation in the National Committee for Quality Assurance (NCQA) Data Aggregator Validation program. This recognition is more than just an accolade; it represents our commitment to providing accurate and reliable clinical data, directly sourced from multiple EHR systems.
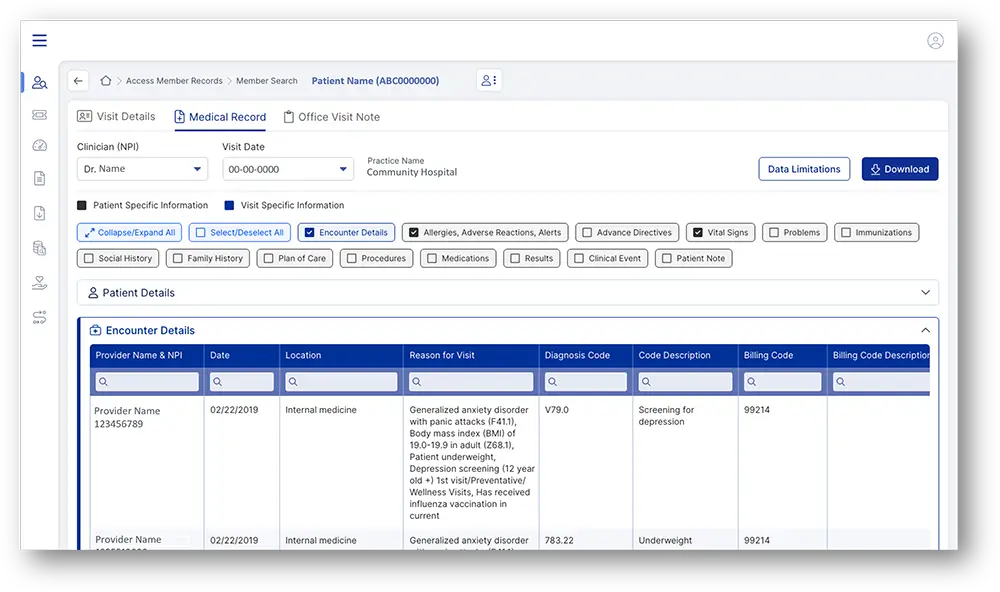
Payers can access longitudinal member records within Exchange Nexus
Exchange Nexus supports over 1000+ discrete elements and can also bring in unstructured data from clinical notes. Payers can view encounter data, procedures, family history, and more all in one place.
Additional Benefits:
- Easily create a clinical data repository for all member visits to in-network providers for longitudinal data analysis.
- Get a 360-degree view of members in-network across providers and periods, standardizing longitudinal member records.
- Scalable clinical data acquisition and exchange powers a range of use cases such as HEDIS supplemental data, Risk Adjustment, payment audits, and population health management.
- Rapidly ID diagnosis alerts to enable care management teams to quickly intervene with patients.
- Make better-informed decisions about the health of patient populations.
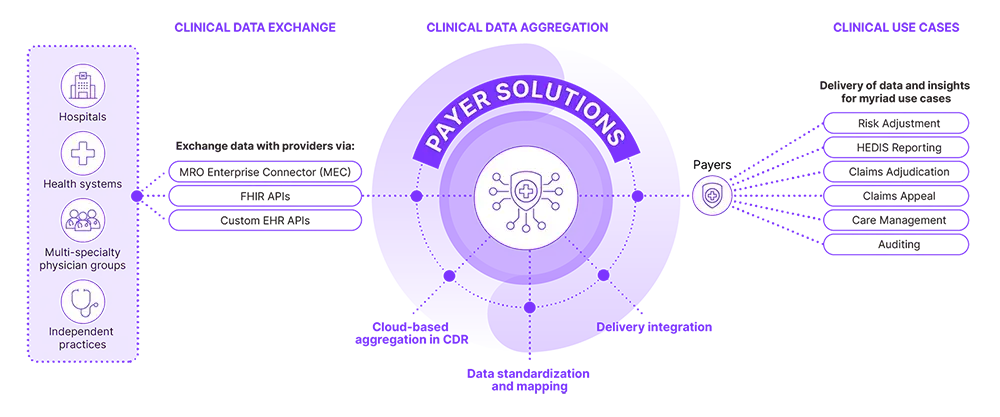
Clinical Data Aggregation and Standardization for Multiple Use Cases
170,000 unique NPIs, across more than 1100 hospitals and health systems, and 35,000+ clinics, including clinicians from 24 unique specialties.
Blueprint for Better Outcomes:
The CareFirst-MRO Partnership Journey
- Reduction of provider participation administrative burden
- Increase of 0.5 STARS, in part due to proven quality improvement
- Improved chart retrieval time from months to 24 hours
- Member’s longitudinal record from multiple EMRs and service locations
- MRO uncovered quality data gaps missed by traditional HEDIS data gathering techniques.
- MRO delivered data outperformed control group data
CASE STUDY
CareFirst BlueCross BlueShield
Learn how MRO and CareFirst partnered to uncover ways to visualize gaps in quality performance, share information, and enhance clinician relationships for insights that drove better patient outcomes.

Achieving better value from the healthcare delivery system is dependent on the secure exchange of actionable data. The work we’re doing with MRO and our healthcare provider partners, aligned with the driving pillar of interoperability for the BlueCross BlueShield Association, is a critical component as we look to drive better outcomes for our patients. When providers have visibility and clinical insights, from both in and out of their network, they have the information needed to facilitate better quality care for their patient populations.
Why Partner with MRO?
Performance
- Cost avoidance for health plans to aggregate EHR data from across a myriad of sources.
- Clinical data aggregation and use of clinical data to reduce provider abrasion as records can be leveraged for multiple use cases.
Interoperability
- Convert structured and unstructured data, such as clinical notes, into a uniform and useable format.
- An ever-growing network of providers, and connectivity with over 250 EHRs, practice management and laboratory information systems
- MRO leverages clinical data exchange services with standardized (FHIR) and proprietary approaches to facilitate a seamless data exchange to acquire enriched, high-value data.
Reliability, Security and Trust
- One of the first vendors to become NCQA Data Aggregator Validated, eliminating the need for primary source verification by CMS for HEDIS supplemental data.
- Over 20 years of experience managing clinical data for providers as a disclosure management organization.
Partnerships are important. Join MRO.
MRO is accelerating clinical data exchange, by ensuring the right information gets to the right place in the right format, on time, every time, enabling health plans to drive better financial outcomes.