As the healthcare landscape continues to evolve, so do the challenges and opportunities presented by CMS’ Quality Payment Program (QPP). Since its inception in 2017, QPP has become increasingly complex, making it harder for providers to avoid penalties and maximize their scores. In the 2024 Performance Year (PY), providers have 199 quality measures available for MIPS (Merit-based Incentive Payment System) and MVP (MIPS Value Pathway) reporting. There are 172 MIPS CQMs (Clinical Quality Measures) and 45 eCQMs (electronic Clinical Quality Measures). Notably, 26 measures can be reported using both collection types—eCQM and MIPS CQM.
The Importance of Quality Measures in 2024
With the Quality Performance Category accounting for 30% of the total composite score in 2024, a strategic approach is more critical than ever. This blog will help you navigate the intricacies of MIPS (Merit-based Incentive Payment System) and MVP (MIPS Value Pathway) reporting to boost your quality scores.
Early analysis of these measures is essential for selecting those that will maximize your quality scores.
Understanding Historical Benchmarks
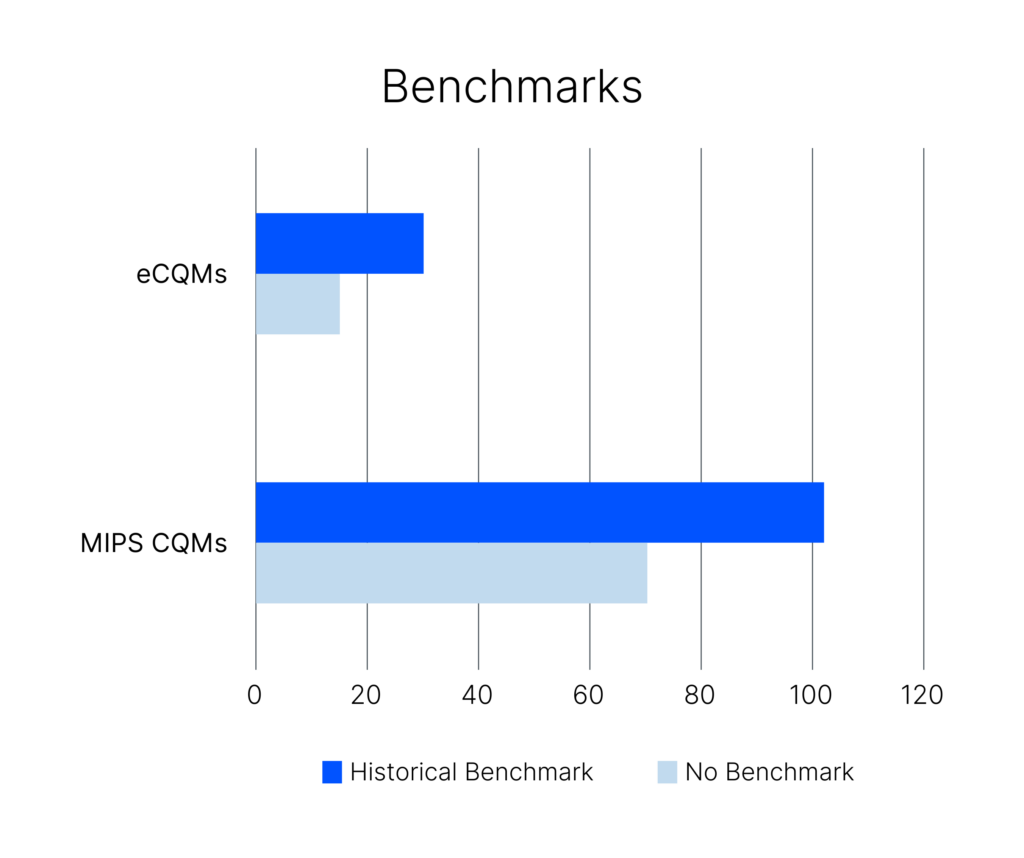
Among the 172 MIPS CQMs, 70 measures lack historical benchmarks, resulting in a minimum score. Exceptions include 11 new measures in 2024 with a 7-point floor and 8 measures introduced in 2023 with a 5-point floor. Reporting measures without benchmarks typically results in lower scores (0-3 points). Similarly, 16 of the 45 eCQMs lack benchmarks and contribute minimally to the Quality Category score.
Avoid measures without historical benchmarks unless they are new measures with higher point floors.
The Advantage of New Measures
Reporting newly introduced measures can be beneficial for several reasons:
- They generate higher scores (7 or 5 points).
- Adequate data submission can establish performance year benchmarks, potentially converting them to historical benchmarks in future years.
Prioritize new measures to maximize scores and establish benchmarks for future performance periods.
Topped-Out Measures: A Closer Look
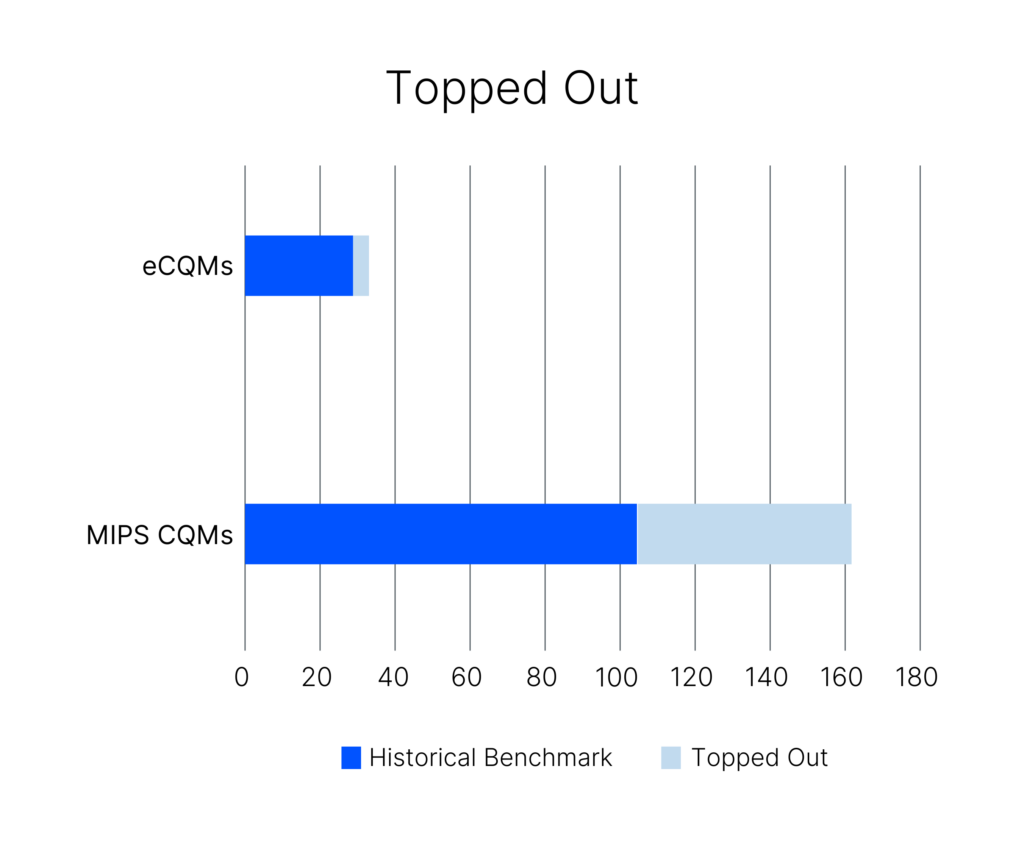
Topped-out measures, particularly those with a 7-point cap, require special attention. Of the 102 MIPS CQMs with historical benchmarks, 59 are topped out, with 48 having a 7-point cap. This means even perfect performance will only generate 7 points, not 10. Among the 29 eCQMs, 3 are topped-out, and 2 have a 7-point cap.
Be cautious with topped-out measures, as they limit scoring potential even with perfect performance.
Choosing Between MIPS CQMs and eCQMs
There are 26 measures that can be reported as either MIPS CQM or eCQM. A detailed comparison of these measure benchmarks can help you make an informed decision. For instance, for QPP 317, scoring 10 points is easier with the eCQM (10th decile ≥ 40.80) compared to the MIPS CQM (10th decile = 100).
Analyze benchmarks closely to decide between MIPS CQMs and eCQMs for optimal scoring.
MIPS vs. MVPs: Making the Right Choice
The aim of the evolution of QPP is to make reporting more meaningful to the providers and reduce the burden of reporting.
MVPs are designed for specific specialties or diseases, offering a more tailored approach. Often, the MVP measure set is a subset of the MIPS measures selected by registries. Comparing MIPS and MVP scores can help identify the best possible scoring strategy for the Quality Category.
Consider MVPs for a more focused reporting experience.
Take Control of Your Quality Score
Navigating the complexities of MIPS and MVP reporting requires a strategic and informed approach. By understanding the importance of historical benchmarks, the benefits of new measures, and the implications of topped-out measures, you can significantly improve your quality category scores in 2024.
We suggest you begin your measure analysis early, prioritize new and high-scoring measures, and carefully compare MIPS and MVP options. Still stuck? Reach out to MRO for personalized guidance.
The above blog post contains research and contextual conclusions provided by Ranu Ray, CMS Research Business Analyst.